I want to talk about depression.
I mean, I want to talk about ADHD. And also depression.
This will be long, but if you struggle with “atypical depression” or find yourself relating to parts of the story below, I hope it may be helpful.
[Disclaimer: I am not a doctor. I’m writing from a combination of personal experience and my own reading and research on the subject of depression.]
1. Escape
Say you’ve been feeling down and unmotivated, you’re having trouble getting out of bed in the morning, and sometimes even basic hygiene can be a struggle. Say you’ve noticed that you seem anhedonic, that is, you’re unable to find real pleasure in just about anything in life. On a scale of 1-10, your mood may have periods where it swings down to 2 or 3, but it’s impossible to swing up past a 5 or 6. Say you feel that that life is simply too much, and you’re incapable of handling the demands it places on you.

This is not a tolerable state to be in. Life has become unpleasant enough that your brain automatically begins looking for an escape as a way to cope with the otherwise unbearable weight of it all. You may find yourself bingeing netflix and youtube, getting high or drunk every night, playing video games for 6+ hours, living on junk food, or simply “doomscrolling” in bed until 2am. Any low effort, low reward kind of activity will do, really.
Let this go on long enough, and you may even find yourself with an actual addiction or eating disorder. If you’ve been completely unable to function, you may have lost your job. Or maybe the fear of being fired just barely keeps you going, but always dependent on the escape, in a never-ending purgatory of anxiety and numbness.
2. Literally me
I’m going to drop the annoying 2nd-person narration and tell you exactly what happened to me, fourteen years ago, when I walked into my doctor’s office and said “I think I might be depressed.”
What happened was this: I was given a questionnaire, Patient Health Questionnaire 9 (PHQ-9), and told, “Please fill this out.”
I suspected I was mildly depressed, but I was also confused because most descriptions of depression I read online didn’t sound exactly like me. However, my responses to the questionnaire indicated that my depression was “severe”, with a provisional diagnosis of major depressive disorder (MDD). The same day, my primary care doctor prescribed Prozac (generic: fluoxetine) and sent me home with a list of therapists I could reach out to, if I felt like it.
Unfortunately for me at the time, this was my first experience with seeking help for a mental health issue, so I didn’t realize just how badly this was going. I’ll summarize the next ten years to save you some time:
- A month of Prozac did nothing, so I was switched to Wellbutrin (generic: bupropion). I noticed an immediate energy boost and my therapist/prescriber kept me on this for the next decade. The energy boost was nice, but after a short period of time I became tolerant and the effect was much smaller.
- Initial bloodwork showed vitamin D insufficiency, so I started supplementing.
- One time when nothing was seeming to work, we tried adding Cymbalta to the mix (generic: duloxetine), but it didn’t do anything noticeable.
- Weekly talk therapy sessions applying cognitive-behavioral therapy (CBT) and some generic psychoanalysis. I filtered for therapists who use CBT because I understood this method had actual scientific evidence. We worked on pragmatic steps I could take toward certain life goals, which were sometimes able to get results on those life goals, but despite outward progress, I remained miserable.
The entire time, the missing puzzle piece that would pull my story together was never noticed, even though the symptoms were in plain view.
3. What’s the Differential?
Did you catch the phrase “provisional diagnosis” mentioned the PHQ-9 above? A nine-question survey score can only be a starting point, not a conclusion. It says there’s something going on here, but it’s not specific enough to narrow down to a single diagnosis.
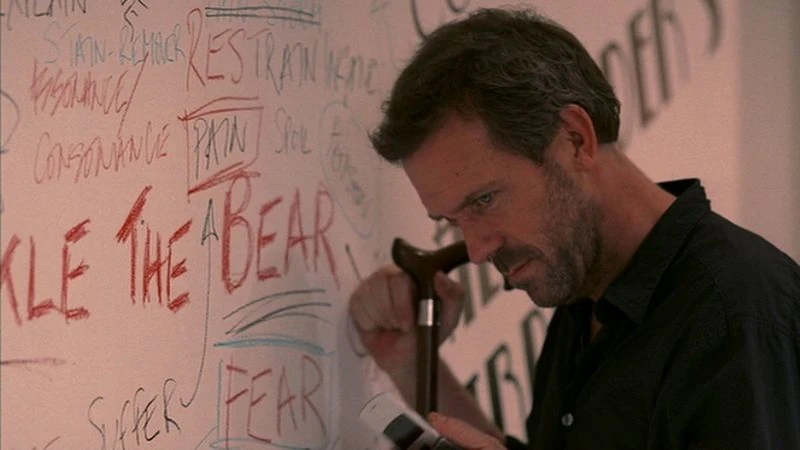
Now, of course I’ve binged every season of House, M.D. (see “Escape” above). I know what a differential diagnosis is:
a systematic process used to identify the proper diagnosis from a set of possible competing diagnoses 1
Once you have the “depression” lens on, it’s easy to ignore the clues that something else is going on. Here’s a non-exhaustive list of things I brought up in talk therapy:
- Low energy, fatigue
- Irritability
- Feelings of guilt and worthlessness
- Difficulty concentrating
- Circadian disorder (delayed sleep phase)
- Impulsiveness, lack of self-control or “willpower”
Several of these are straight out of the DSM 5 criteria for MDD, but there are some that should raise eyebrows. Irritability, difficulty concentrating, impulsiveness are also diagnostic criteria for ADHD.
In the National Comorbidity Survey Replication (NCS-R) performed in 2004, it was found that having ADHD increases your odds of having major depression by a factor of nearly 3x.2 Subjectively, it’s not that hard to see how being unable to live up to the standards set by schools, colleges, and workplaces could lead to feelings of worthlessness and guilt.
Circadian disorders are also a common comorbidity of ADHD:
DSPS and late chronotype are frequently comorbid in adults and adolescents with ADHD. The pathophysiology linking ADHD and CRSD maybe both behavioral and biological. Deficits in impulsivity control may affect the ability of an individual to settle down, leading to bedtime resistance and resulting in delayed sleep onset. In addition, it is proposed that individuals with ADHD may have a stronger circadian evening preference and possible endogenous melatonin increase delay.3
We’re even learning that (perhaps counterintuitively) fatigue can be a symptom of adult ADHD.4
Finally, consider that Prozac, an SSRI, did nothing for me, while Wellbutrin, a dopamine-reuptake inhibitor, did help, at least a little.
It looks like I might have been struggling with undiagnosed and untreated ADHD my entire life. Personally, I never even considered it, because my pop-culture understanding of the condition was so caricatured and limited. It didn’t occur to me I might have it until many years later.
4. Invisible
Who else is living with undiagnosed, untreated ADHD right now?
Adult ADHD appears to be fairly prevalent in the general population (2.5%–5%) and is progressively increasing5
What are the more visible conditions they may be diagnosed with instead of ADHD?
Common psychiatric comorbidities are depression, substance use disorders, generalized anxiety disorder, social phobia, specific phobia, panic disorder, bipolar disorder, dysthymia, obsessive-compulsive disorder, intermittent explosive disorder, and eating disorders. Among personality disorders, borderline, histrionic, narcissistic, and antisocial personality disorders are commonly comorbid. In the arena of medical comorbidities, hypertension, type II diabetes, obesity, asthma, and migraine are common.5
Are you struggling with depression or anxiety? Or maybe addiction? Social phobias? Eating disorders? Have you considered whether ADHD may be part of the story?
5. The ADHD Tax
If you’ve ever heard from people with ADHD, you might have heard of the “ADHD tax”, that is, additional costs incurred because you are a person with ADHD. This might be something like late fees and interest payments on overdue bills or missed opportunities because of application deadlines. Even these examples can feel pretty brutal, but the following three paragraphs from a paper by Katzman, et al put it even more starkly:
Adult ADHD is associated with profound functional and psychosocial disability, leading to serious personal and societal costs. Its most prominent feature is attentional dysfunction, associated especially with impairment in focused and sustained attention [21]. Individuals with ADHD also experience neuropsychological difficulties associated with deficient inhibition [22], memory [22], executive functioning [23, 24], decision making [25], and emotional dysregulation [26]. Adult ADHD can have negative consequences for individuals’ self-esteem and the quality of interpersonal relationships, with both colleagues and significant others [27, 28]. For example, in a community sample of 1001 adults, those with ADHD were significantly more likely to have been divorced (28% vs 15% controls, P ≤ 0.001) and were significantly less satisfied with their personal, social and professional lives [29]. ADHD is associated with educational difficulties, requiring extra help, attending special classes, repeating grades [30], as well as higher rates of academic suspension and drop outs [31]. College students with ADHD have reduced grade point averages and are less likely to graduate than students without ADHD [32]. Later in life, adults with ADHD experience challenges with time management, organization, and self-regulation, which can result in employment and financial problem [27, 33]. One study estimated the individual income reduction in adults with ADHD in the United States to be between $8900 and $15,400 annually [34].
The detrimental effects of ADHD on overall health and safety provide additional imperative to appropriately recognize and manage this debilitating disorder. Adult ADHD has been associated with poorer driving and a higher incidence of traffic citations and motor vehicle accidents [35]. A recent study found that Japanese adults with ADHD visited physicians 10 times more often than a non-ADHD control group, and had rates of emergency room visits and hospitalization three times greater than controls [28]. Individuals with ADHD in Denmark have a lower life expectancy and more than double the risk of death than adults without ADHD [36]. This was mostly attributed to accidental death and characteristics associated with ADHD such as risk-taking behaviour.
In addition to its substantial burden at the individual level, adult ADHD is often associated with considerable societal costs. Notably, there have been consistent associations between adult ADHD and unemployment [34, 37]. In one study, adults with ADHD were 42% less likely to be employed full-time as were adults without ADHD (rates of full-time employment: 34% vs 59%, respectively, P < 0.001) [34]. The associated loss of workforce productivity has been estimated to cost $67 to $116 billion annually in the United States alone [34]. A more recent study estimated the overall annual cost of ADHD in the United States at between $143 and $266 billion, largely due to productivity and income losses [38]. ADHD has been associated with increased criminality [39], with one study reporting that 47% of patients with ADHD had at least one criminal sentence [4]. Another study estimated the prevalence of ADHD among long-term inmates of a prison at 40% [40].6
These are heavy consequences of an undiagnosed developmental disorder. I recognize enough of them in myself, and it honestly helps the healing process to be able to attribute my differentness to a specific condition. And on the whole, I think I’m one of the lucky ones who turned out with a fairly “normal” looking life. It’s not hard for me to imagine another version of myself who was a failure to launch, struggled to find love or work or meaning, or ultimately gave up on it all.
In the end, as a result of my introspection and my own research, I walked into another doctor’s office and said “I think I might have ADHD.” The result of taking that step was life-changing. It shouldn’t have to take 43 years to figure it out, but at least I am now being treated and I’ve already seen more positive changes in my life than with 12+ years of treatment focused on depression alone.
6. Where to now?
Our understanding of ADHD is still relatively poor. It’s often considered mainly an issue of childhood. In fact, a key diagnostic criterion is that it occurs in childhood, to the point where if you are a smart person who did well in school despite significant inattentiveness, you will probably not be diagnosed with ADHD. Even if it’s a significant challenge for you to perform at the level expected, say, in grad school or in your career as an adult, it may be difficult to get a doctor to recognize it as ADHD.
ADHD is still relatively new as a diagnosis. Stumbling blocks and uncertainties abound:
- Your doctor or therapist may hold antiquated views about ADHD (“it’s just fidgety kids who need to develop discipline”).
- Despite a widespread dismissiveness that “everyone has ADHD these days”, ADHD in adults still generally goes undiagnosed.
- ADHD has a ton of documented comorbidities and may be a causal factor in those cases, but the other condition(s) may be diagnosed first, leaving you confused.
- Even when doctors take it seriously, they may have an imperfect understanding of the various ways in which ADHD presents.
- Causality is incredibly hard to pin down in cases of multiple comorbid psychological conditions. Instead of one-way causation, we’re likely to find feedback mechanisms between them. Practically speaking, look for actions you can take that help across the board, or on the symptoms that cause you the most impairment.
Finally, I don’t think it’s widely considered possible that ADHD can be induced in an otherwise healthy brain through bad habits alone, but we seriously consider (and study) this possibility. I don’t think ADHD is a binary condition, that either you have it or you don’t. We can train our brains to require more and more novelty every day by consuming social media during every dull moment. While the research on this is currently limited, I suspect the result of saturating your dopamine-reward system with continuous stimulation may very well resemble ADHD. It may also lead to anhedonia, a main feature of depression, along with a host of potential consequences listed above.
Thanks for attending my TED talk. In future posts, I plan to talk more pragmatically about what we can do with what we know about all of this. It won’t be limited to ADHD, of course, because I do really have lifelong struggles with depression and I’m working my way through that, too. But I’ll spend less time quoting studies and more time sharing what wisdom I feel I have found.
References
-
Cook CE, Décary S. Higher order thinking about differential diagnosis. Braz J Phys Ther. 2020 Jan-Feb;24(1):1-7. doi: 10.1016/j.bjpt.2019.01.010. Epub 2019 Jan 30. PMID: 30723033; PMCID: PMC6994315. ↩︎
-
Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, Faraone SV, Greenhill LL, Howes MJ, Secnik K, Spencer T, Ustun TB, Walters EE, Zaslavsky AM. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006 Apr;163(4):716-23. doi: 10.1176/ajp.2006.163.4.716. PMID: 16585449; PMCID: PMC2859678. ↩︎
-
Wajszilber D, Santiseban JA, Gruber R. Sleep disorders in patients with ADHD: impact and management challenges. Nat Sci Sleep. 2018 Dec 14;10:453-480. doi: 10.2147/NSS.S163074. PMID: 30588139; PMCID: PMC6299464. ↩︎
-
Rogers DC, Dittner AJ, Rimes KA, Chalder T. Fatigue in an adult attention deficit hyperactivity disorder population: A trans-diagnostic approach. Br J Clin Psychol. 2017 Mar;56(1):33-52. doi: 10.1111/bjc.12119. Epub 2016 Dec 5. PMID: 27918087. ↩︎
-
Prakash J, Chatterjee K, Guha S, Srivastava K, Chauhan VS. Adult attention-deficit Hyperactivity disorder: From clinical reality toward conceptual clarity. Ind Psychiatry J. 2021 Jan-Jun;30(1):23-28. doi: 10.4103/ipj.ipj_7_21. Epub 2021 Jun 10. PMID: 34483520; PMCID: PMC8395556. ↩︎ ↩︎
-
Katzman MA, Bilkey TS, Chokka PR, Fallu A, Klassen LJ. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry. 2017 Aug 22;17(1):302. doi: 10.1186/s12888-017-1463-3. PMID: 28830387; PMCID: PMC5567978. ↩︎